Please scroll on the PDF below to view the entire document!
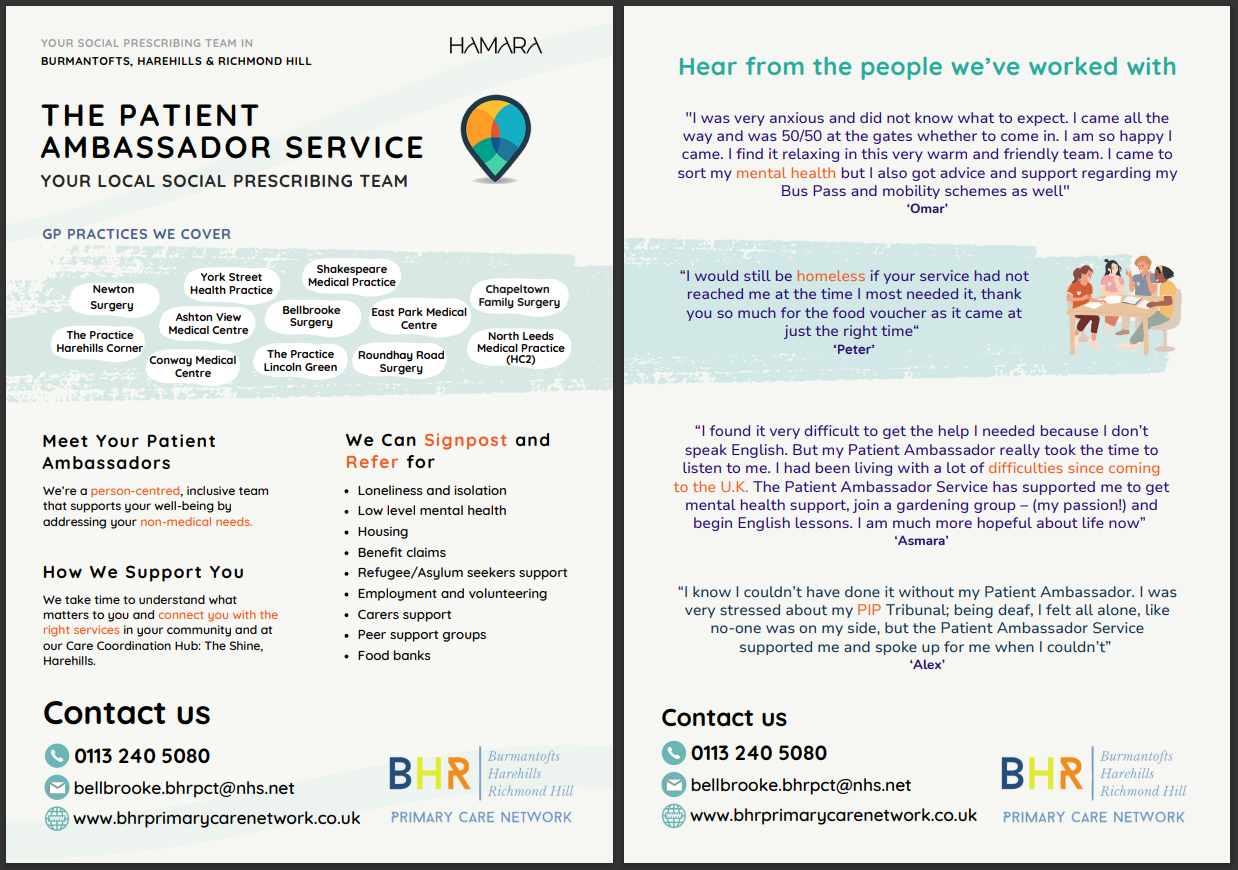
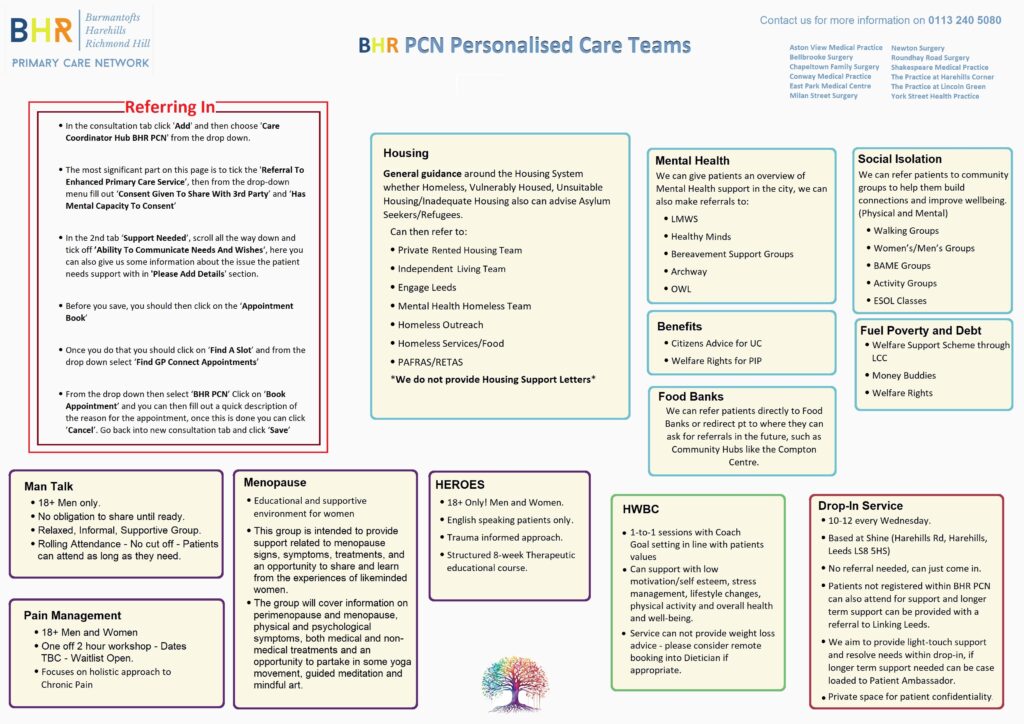
Social Prescribers
How we can help.
- Help and support with non-medical issues e.g. housing, debts, mental health, bereavement, refugee/asylum seeker issues and benefits.
- Support clients to access Health & Social Care where needed. This will include supporting patients at meetings and acting as advocates.
- Offer peer support groups e.g. sleep well and mental health
- Work with other third sector organisations in the community to break down barriers for patients and help them to access information they need.
- We offer open ended support and spend time one-to-one actively listening and exploring what matters most to patients.
- We connect patients to local specialist services that can meet their non-medical needs such as inadequate housing, low-level mental health, language barriers, social isolation, benefits advice, food/fuel poverty and much more.
- We deliver group work and peer support programmes, taking the support out of the four walls of the clinical room, working towards reducing social isolation through bringing people together with shared experiences
How we can help.
- To assess patients with soft tissue, muscle and joint pain and to decide on the most appropriate management pathway.
- FCPs are physiotherapists with expertise in the assessment and management of Musculoskeletal (MSK) conditions.
Routine steroid injections can be administered to certain joints e.g. knee, shoulder. However, there are some joints which CANNOT be administered; hip, elbow, small hand joints and spinal.
Leeds Mental Wellbeing Service (LMWS)
How we can help.
- We address the mental health needs of patients with complex histories, co-morbidity, patients who haven’t previously met criteria for or have disengaged with IAPT or CMHTs.
- Support patients who find it difficult navigating into mental health services by themselves.

Trauma Informed Approach
Trauma Charter
As a PCN, we are committed to implementing trauma informed care and agree to the commitment described in the charter.
Healthy Minds
Healthy Minds appointments are available Monday – Friday during core hours. These appointments support patients who are struggling with low level mental health and emotional wellbeing difficulties.
DO NOT BOOK under 18s, patients who are expressing thoughts of self-harm, or patients who are under the secondary care mental health team. Any questions reach out to teresa.dcaccia@nhs.net.
PLEASE ALWAYS DOUBLE UP THE APPOINTMENT FOR PATIENTS NEEDING LANGUAGE LINE OR INTERPRETATION FROM A FAMILY MEMBER
HEROES Programme
The HEROES programme is a nine-week, 20-hour therapeutic group work programme which has been available to patients at GP practices within the Burmantofts, Harehills and Richmond Hill (BHR) areas, called ‘Primary Care Networks’ (PCN) since 2020 – and has reported some impressive results.
HEROES is based on supporting people to shine a light on, and shift, any limits they have created about themselves and their identity in response to trauma they may have encountered in their lives.
The programme holds a safe space for all to build a better relationship with themselves and the world around them, for effective healing to occur.
It focuses on the body as well as the mind, exploring nervous system regulation and physical responses as well as emotional support such as self-compassion, self-identity and inner-forgiveness.
HEROES teaches unique, original, accessible methods and tools to use when suffering, such as The Bridge of Self compassion and our revolutionary SAVE method for inner child healing.
Simply put, above all else, it supports to build a better relationship with YOU in every way and guiding on how to create the changes in life.


How we can help:
- The HEROES Peer Support Programme is a series of courses, workshops and generalised support groups for patients struggling with their mental health.
- HEROES stands for Healing, Education and Recovery Of Emotional Strength and it also stands for the kind of person who joins our groups!
- Groups are run by trained facilitators in a safe, compassionate and recovery-focused space.
We explore topics such as Self-Compassionate practice, Mindfulness, Anxiety Management, Confidence Building and Assertiveness Skills. New courses will be added throughout the year.
Please contact the Care Coordination hub – for further details.
We look forward to welcoming more patients who may be suffering emotionally. All mental health diagnoses welcome!
If you would like to know more about Miranda’s HEROES programme outside of the BHR PCN click on the link below:
The HEROES Groupwork Programme – Miranda Arieh
SMI
BHR PCN have a small team to support patients that have a diagnosis of a serious mental illness (SMI): Schizophrenia, bipolar disorder and other psychoses. Around 400,00 people in England are living with Schizophrenia and around 544,631 people are living with bipolar disorder. People living with a SMI are at considerably increased risk of physical ill health than the general population and have demonstrably poorer health and health outcomes. Our team of healthcare assistants, nursing associates and care coordinators are a dedicate team that are here to help our patients to access primary care services and reduce health inequalities for this population.
The team focus is supporting patients to have annual health reviews which include a physical health check: Bloods test, Blood Pressure, check patients are accessing cancer screening appointments. It also includes a review of their mental health care plans and includes development of personalised care plans. The team do this by assisting patients to seek help with lifestyles changes, emotional support and can support patients in accessing health and wellbeing coaching.
Importance of having a annual health check:
Why is it important for you to attend for your SMI health review
We Offer
- GP appointments:
Monday to Friday, 4:00 pm to 8:00 pm
Saturday, 9:00 am to 3:00 pm
Sunday, 9:00 am to 1:00 pm - Advanced Nurse Practitioner (ANP):
Tuesday and Thursday, 6:00 pm to 8:00 pm
Saturday, 10:00 am to 2:00 pm - Long Acting Reversible Contraception (LARC) coil & implants insertion/removal:
Saturday and Sunday - Practice Nurse:
Saturday, 9:00 am to 3:00 pm
Sunday, 9:00 am to 1:00 pm - Health Care Assistant (HCA):
Saturday and Sunday (limited availability)
How we can help.
- Support practices with medication related process such as medication queries, medication reviews and repeat prescription reauthorisations. Supporting practices with processing clinical documents and structured medication reviews.
- Safety audits including MHRA and amber drug monitoring.
- Project work highlighted by national quality and safety directives.
- Supporting with all aspects of prescribing for the care homes team.

Pharmacy First
The Pharmacy First service builds on the NHS Community Pharmacist Consultation Service which has run since October 2019. The consultation service enables patients to be referred into community pharmacy for a minor illness or an urgent medicine supply.
The new Pharmacy First service, launched 31 January 2024, adds to the existing consultation service and enables community pharmacies to complete episodes of care for 7 common conditions following defined clinical pathways.
Accessing Pharmacy First services
The following table shows the 7 conditions pharmacists can manage across various age ranges.
| Clinical pathway | Age range |
| Acute otitis media* | 1 to 17 years |
| Impetigo | 1 year and over |
| Infected insect bites | 1 year and over |
| Shingles | 18 years and over |
| Sinusitis | 12 years and over |
| Sore throat | 5 years and over |
| Uncomplicated urinary tract infections | Women 16-64 years |
* Distance selling pharmacies will not complete consultations for acute otitis media.
Patients will be able to access the 7 clinical pathways element via referrals from referring organisations including general practice, urgent and emergency care settings, and NHS 111 (online and via telephone). In addition, for the 7 common conditions clinical pathway consultations only, patients can access the service by attending or contacting the pharmacy directly without the need for referral.
What happens next?
If you are being referred to your local pharmacy for other minor ailments *not one of the common conditions shown above. We will send your details and information about your condition to the pharmacy you have chosen.
You should call the pharmacy a few hours after you have been referred (if they haven’t already contacted you) to discuss next steps advising you were referred from your practice.
You will then have a consultation and be assessed by the pharmacist in a private consultation room.
How will the pharmacist help?
Pharmacists are highly skilled healthcare professionals who have trained for at least five years.
If the pharmacist reviews your symptoms and thinks you need to see another healthcare professional (eg GP, dentist, optician), they will help to arrange this.
The pharmacist can provide advice and reassurance on how to manage your condition, as many minor illnesses get better on their own. If the pharmacist thinks you need treatment to help with your symptoms, they may recommend an over-the-counter medicine.
If you are seeing them because you have run out of your usual medicine, they can help arrange a new supply.
The pharmacist will record the outcome of your consultation and send it to your GP to ensure your GP record is updated, including if any medicines are supplied.
Which pharmacy can I go to?
You can choose which pharmacy you go to, as long as it’s taking part in the scheme.
How will we use your information?
We will only use your personal information to help manage your care safely.
All of your personal information will be held securely by the NHS and will not be shared with third parties.

Health and Wellbeing Coaches
What is a Health and Wellbeing Coach?
A health and wellbeing coach can support you to improve how you manage your physical and mental health. They work with you through a series of sessions to help achieve your personalised health and care plan goals, offering support and advice about diet and lifestyle.
How can a health and wellbeing coach support me?
Health and wellbeing coaches support you to take proactive steps to improve the way you manage your physical and mental health conditions based on what matters to you.
They support you to develop knowledge, skills and confidence in managing your health and care, to improve your health and quality of life. They will coach and motivate you through multiple sessions to identify your needs, set goals and support you to achieve your personalised health are care objectives – providing interventions such as self-management education and peer support.
- 1:1 and group coaching
- Support setting personalised health goals
- Linking in with other services
- Support to manage your long-term health condition
- Support towards eating well, staying active or managing your weight
- Support to manage your mental wellbeing
- Adhere to a care plan
Where is a health and wellbeing coach based?
Health and wellbeing coaches are based within your local community. They work out of local GP surgeries so you may have an appointment at a different surgery to where you are registered.
How do I make an appointment to see a health and wellbeing coach?
Health and wellbeing coaches are accessible via your GP Surgery, when ringing for an appointment the reception team may suggest you speak to a health and wellbeing coach and a member of the team will then be in touch with more information and to find out if health coaching will be suitable for you. You can also make a self-referral by calling 01132405080.
What can I expect from an appointment with a health and wellbeing coach?
During the first session with a health and wellbeing coach they will find out more about you, your lifestyle, values, goals and anything that might get in the way of achieving those goals. You will then set some short-term goals that will enable you to start to work towards what it is you want to achieve. In the sessions that follow you will review your progress, set new goals and discuss any challenges you might have faced to help you overcome these in the future. In doing so, health coaching helps you develop the skills and confidence to manage your health and wellbeing.
Will I need to see a health and wellbeing coach on a regular basis?
You will be offered 6-8 sessions of support, consisting of 45-minute consultations via telephone, online or face-to-face.
Why is the health and wellbeing coach based at my GP surgery?
Primary care networks are prioritising the need for dedicated health and wellbeing provision within their primary care teams. The health and wellbeing coach works closely with the clinical staff in your GP practice to seek advice and guidance on different aspects of your care where necessary.
Health Population Management Hub

Around 20,800 people are diagnosed with cancer each year in Leeds and 55% of cancers are diagnosed early. Early diagnosis saves lives but screening uptake for breast, cervical and bowel cancers is often low. So, cancer screening is an important priority for our PCN.
Cancer screening participation varies depending on multiple demographic and geographical factors.
What we know:
- Participation in bowel screening is low in deprived areas, and particularly South Asian communities.
- Participation in cervical screening is low in deprived areas, however there is variation in rates between ethnic groups.
- Breast screening is lowest in deprived areas and people from Black or South Asian backgrounds.
We want to support our patients to feel empowered to access cancer screening services. We have a wide variety of resources available and want to make our patients feel comfortable and reassured to enable participation in cancer screening.
Cervical screening – Leeds Health and Care Partnership
If you think you are eligible and due one of the cancer screening tests please contact your GP surgery who can advise further.
BHR PCN have a small dedicated team of healthcare assistants, nursing associates and care coordinators. They provide support to practices to identify and coordination care for a range of people, particularly those with long-term conditions and multiple long-term conditions. The team help people co-ordinate and navigate their care across the health and care system.
The approach is to provide support and influence the health of the community and its patients to tackle health inequalities.
Our population have a higher prevalence of long-term conditions particularly at an earlier age and because of the nature of our more deprived communities, along with our culturally diverse population, these multimorbidity patients are typically our hard-to-reach patients.
The team objectives is to support patients to stay well and manage their condition by working very closely with their GP’s.
Our Priority is Diabetes

What is diabetes? Find out in our two-minute video spoken in English. link: https://youtu.be/ZLOjD5IfUyU
Or choose a version in Urdu, Gujarati, Punjabi or Sylheti from our https://www.youtube.com/playlist?list=PLQDlTVSOXD9GeCq19dVbUpYZewQaztdsR
Our Focus area
Type 2 Diabetes in the Young Initiative
The National Diabetes Audit (NDA) shows that prevalence of type 2 diabetes in younger people is increasing yearly, with an estimated 137,260 people with type 2 diabetes aged 18-39 in England. In west Yorkshire prevalence is estimated at 7500 people; the majority of whom are cared for exclusively in General Practice (GP).
Diabetes in younger people is associated with a more aggressive diabetes phenotype than older-onset type 2 diabetes, including more rapid progression of glycaemia and early development of complications with significant reduction in life expectancy. Despite this, people with EOT2D are less likely to receive all NICE recommended care processes and tend to have higher HbA1c than older people with type 2 diabetes. The PCN LTC team are focused on supporting practices to target this population and improve health outcomes.
Type 2 Diabetes Path to Remission Programme
The NHS Type 2 Diabetes Path to Remission Programme is a joint initiative between NHS England and Diabetes UK. This programme provides a low calorie, total diet replacement treatment for people who are living with type 2 diabetes and obesity or overweight: the NHS Type 2 Diabetes Path to Remission Programme.
The programme is being offered to eligible people, participants will be offered low calorie, total diet replacement products including soups and shakes consisting of 800 to 900 kilocalories a day for 12 weeks. During this time, participants will replace all normal meals with these products. Alongside this, participants will receive support and monitoring for 12 months including help to re-introduce food after the initial 12-week period. This support will provide participants with the help and advice they need throughout every stage of the programme. The programme is fully funded by the NHS, therefore there is no cost to participants.
NHS Diabetes Prevention Programme
The NHS Diabetes Prevention Programme (NHS DPP) is a joint commitment from NHS England, Public Health England and Diabetes UK, to deliver at scale, evidence based behavioural interventions for individuals identified as being at high risk of developing Type 2 diabetes.
Start Your Journey to a Healther You Leaflet (wypartnership.co.uk) – Urdu
Start Your Journey to a Healther You Leaflet (wypartnership.co.uk) – Punjabi
The Health Population Management Hub
The BHR PCN has a dedicated team of healthcare assistants, nursing associates, and care coordinators who work within the Health Population Management Hub. Their role is to support practices in identifying and coordinating care for individuals, particularly those with, or at risk of, developing long-term conditions. The team helps patients navigate and coordinate their care across the health and care system, aiming to improve the health of the community and reduce health inequalities.
One of the team’s key objectives is to educate and support patients with prediabetes. Prediabetes occurs when blood sugar levels are higher than normal but not high enough for a diagnosis of type 2 diabetes. It is measured using a HbA1c test. This shows your average blood glucose (sugar) levels for the last two to three months.
People with prediabetes are at a higher risk of developing type 2 diabetes but often experience no symptoms. Medical terms for elevated blood sugar include:
- Impaired fasting glucose (IFG)
- Impaired glucose tolerance (IGT)
- Impaired glucose regulation (IGR)
- Non-diabetic hyperglycaemia
This video explains what your HbA1c result means:
Preventing Type 2 Diabetes
Research shows that combining lifestyle changes—such as improving diet, increasing physical activity, and achieving sustainable weight loss (if appropriate) can lower the risk of developing type 2 diabetes by around 50%. Being at risk doesn’t guarantee you’ll develop type 2 diabetes, but you can reduce your risk by making healthier choices in your diet and activity levels. Your healthcare team can support you in making these changes.
Managing Your Weight
If you are overweight or obese and at high risk of type 2 diabetes, even modest weight loss can be beneficial. Losing 5% of your body weight can significantly lower your risk. There are various ways to lose weight, and the key is finding the right support and strategies that work for you. If you need help managing your weight, a dietitian may be able to assist you. Your GP can also direct you to local weight management services.
Eating a Healthy, Balanced Diet
There’s no single “special diet” for people at risk of type 2 diabetes because everyone’s needs are different. However, the types of food we consume play a role in our risk. A diet high in sugar and carbohydrates and low in fibre content, is linked to an increased risk of developing type 2 diabetes. The good news is that by making healthier food choices, you can reduce this risk.
Healthy eating patterns linked with a lower risk of type 2 diabetes include:
- The Mediterranean diet – Mediterranean meal plan | Diabetes UK
- The Dietary Approaches to Stop Hypertension (DASH) diet – DASH diet – healthy eating that helps lower blood pressure
- Vegetarian and Vegan diets – The vegetarian diet – NHS / The vegan diet – NHS
- Reduced carbohydrate – Low-carb diet and meal plan | Eating with diabetes | Diabetes UK
These eating patterns emphasise healthy foods like fruits, vegetables, whole grains, and lean proteins. It’s the overall balance of your diet that plays a crucial role in keeping you healthy. To reduce your risk, aim to eat more foods linked with a lower risk, such as:
- Fruits and vegetables
- Whole grains (brown rice, wholemeal bread and whole wheat pasta)
- Beans and legumes
- Nuts and seeds
- Dairy e.g. Natural (Greek) yogurt and cheese
- Lean proteins (chicken, turkey) and fish
- Water, tea and coffee (unsweetened)
At the same time, reduce the intake of foods that are linked to a higher risk of type 2 diabetes, such as:
- Sugary drinks
- Red and processed meats (like beef, lamb, pork, ham, and sausages)
- Refined carbohydrates (such as sugary snacks, crisps, white bread, white rice, white pasta and sugary cereals)
- Potatoes (particularly French fries)
Be More Active
A sedentary lifestyle—spending long periods inactive—has been linked to an increased risk of type 2 diabetes. Increasing physical activity in your daily life can help lower your risk. You don’t have to join a gym or start a new sport. Small changes can make a difference. Try standing while taking phone calls, using stairs instead of the lift, doing chair exercises, or taking a walk during your lunch break.
By incorporating these small changes into your routine, you can make a big impact on your health and reduce your risk of type 2 diabetes.
NHS Diabetes Prevention Programme
The NHS Diabetes Prevention Programme (NHS DPP) is a joint commitment from NHS England, Public Health England and Diabetes UK, to deliver at scale, evidence based behavioural interventions for individuals identified as being at high risk of developing Type 2 diabetes.
Click here for more information – NHS Diabetes Prevention Information
Start Your Journey to a Healthier You Leaflet (wypartnership.co.uk) – Urdu
Start Your Journey to a Healther You Leaflet (wypartnership.co.uk) – Punjabi
Prediabetes Workshops
In addition to the NHS Diabetes Prevention Programme, the team will be running regular dedicated workshops aimed at patients who have been informed they have prediabetes in the last 12 months. These small group sessions will provide individuals with information about managing blood sugar levels alongside practical dietary and lifestyle advice. If you are interested in attending one of our workshops, please contact: 07355 674627
Appointment reminders for childhood immunisations are now also being used across the PCN in a number of different languages – for more information please select:
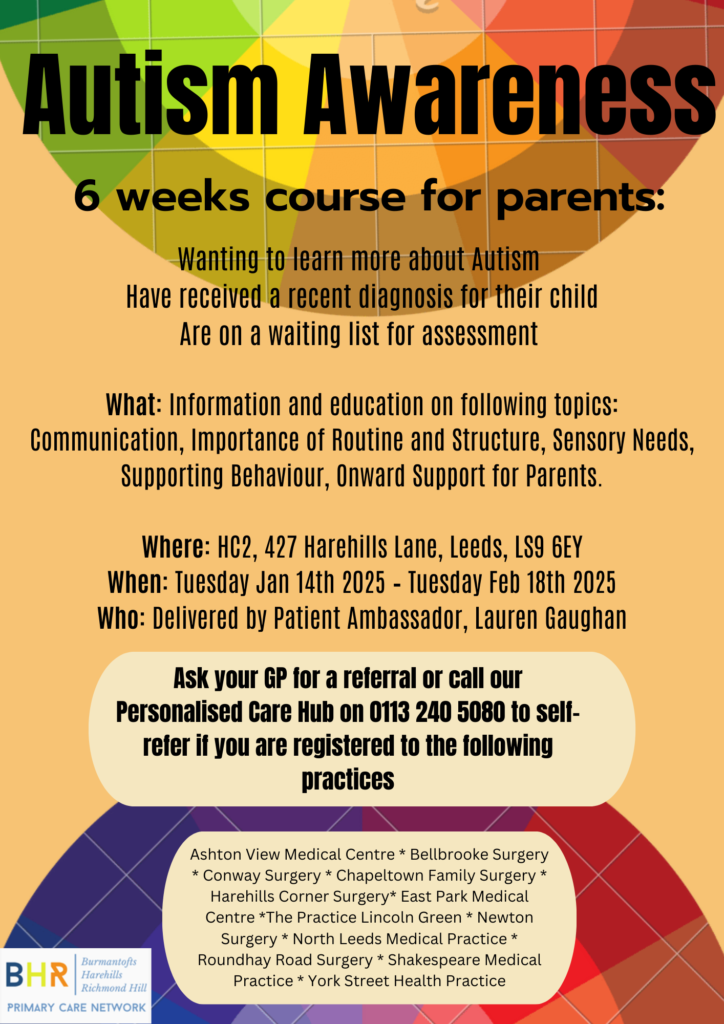
Children and Young People’s Social Prescribers
How we can help.
- Help and support with non-medical issues e.g., mental health, low school attendance, bullying, Primary School to High School transitioning, young carer support, managing challenging or risk-taking behaviour, NEET support (Not in Education, Employment or Training), Engaging patients with high repeat DNA’s where their health may be affected.
- Information on parent skills and classes
- Support with general well-being
- Digital Literacy support and SEND guidance.
- Support clients to access Health & Social Care where needed. This will include supporting patients at meetings and acting as advocates.
- Work with other third sector organisations in the community to break down barriers for patients and help them to access information they need.
Please refer through the orange triangle on the Child Health Hub tab.
Women’s Health Clinic
The Women’s Health Hub for Leeds has continued to expand work within the PCN. We are collaborating with Dr Chipeta gynaecology consultant at LTHT to offer outreach clinics to PCN patients referred to LTHT gynaecology services, offering faster access to gynaecology advice, treatment and if required referral for surgical interventions. This has enabled women in our PCN to be seen at around half the standard waiting time for gynaecology compared to that experienced for the rest of the city population.
We are able to offer a bi-monthly Women’s health lunch and learn & MDT for our PCN clinical teams lead by Dr Chipeta and Dr Spencer (clinical lead for menopause) which offers learning around different women’s health conditions and discussion and advice on complex patient cases.
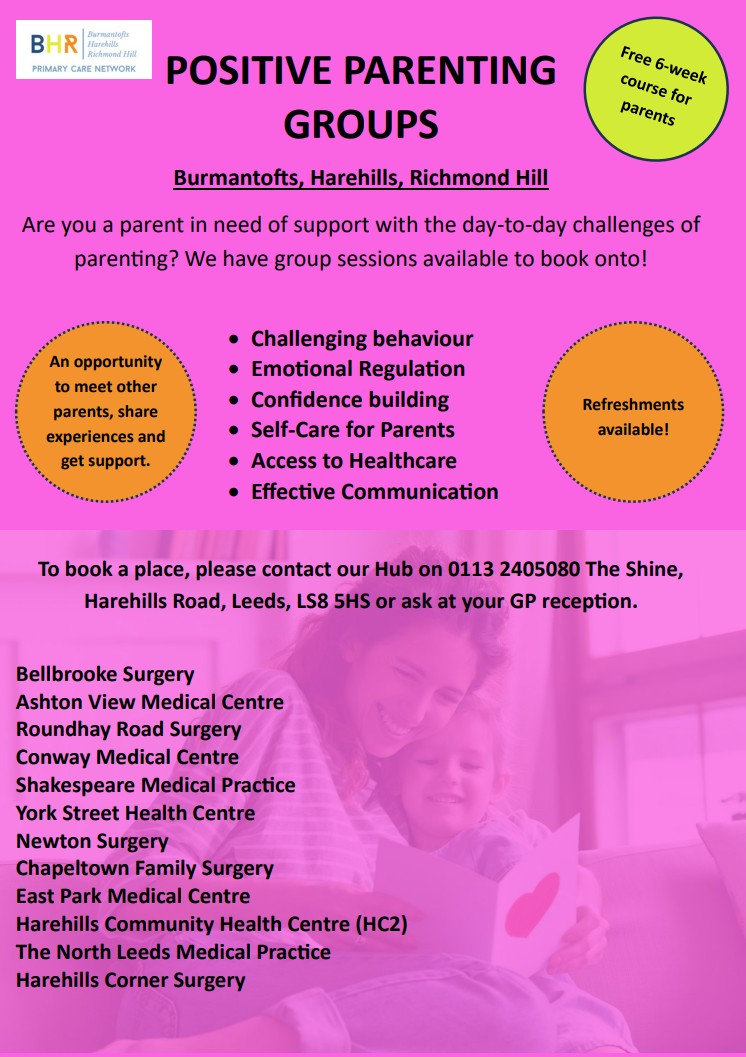
Education and support groups
As a PCN we are also able to offer support and education sessions to patients enabling women to access programmes focusing on menstrual health, PCOS, PMS/PMDD, endometriosis and menopause.
We would welcome any patients wishing to access these groups to contact their GP practice for a referral to be processed.
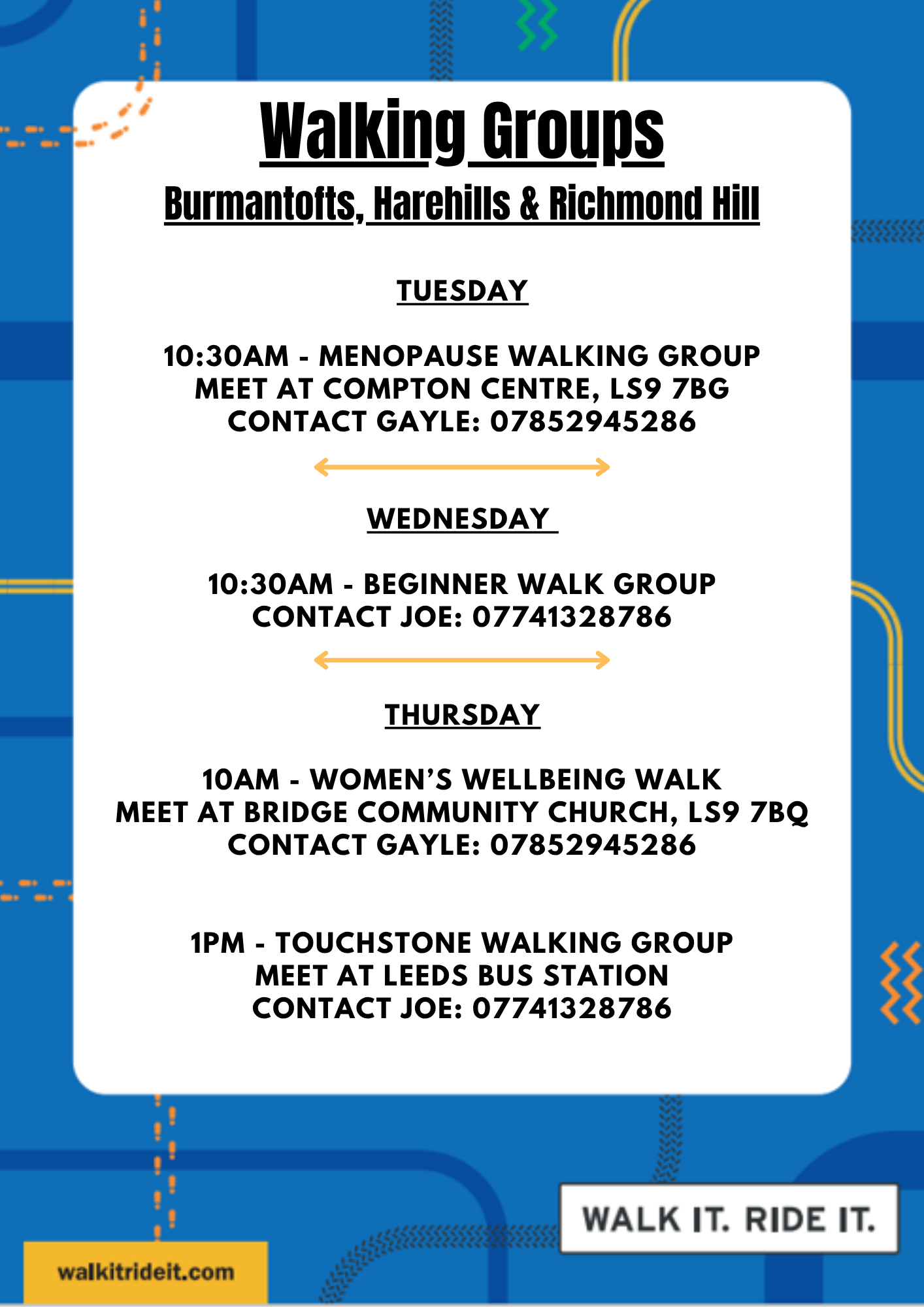
Walk It Ride It – Leeds
We’re making it easier for people to try free walking, wheeling, and cycling activities in Burmantofts, Harehills, and Richmond Hill.
Interested in cycling or walking more?
Spending time outside and moving around can help improve our mood, lower stress, and make us feel more relaxed.
Visit their website here for more information

The annual Learning disability health check was introduced into Primary care in 2006, The primary purpose of annual health checks is to address access and barriers experienced by people with a Learning Disability, furthermore, to allow the identification of unmet health needs. Health checks aim to improve prescribing and co-ordination with secondary care and identify any reasonable adjustment in accordance with the Disability Discrimination Act 1995.
People with a learning disability have poorer health and a lower life expectancy than the general population. They may not recognise that they are unwell or may be unable to communicate how they feel. They could also develop conditions or face challenges that are associated with their learning disability. The annual health checks for people with a learning disability differ from NHS health checks and include a more specific and detailed examination of a person’s physical and mental health. Carrying out these checks ensures that health issues are identified early, support can be provided promptly, and their health action plan is up to date.
Who is eligible?
Only patients with a diagnosed Learning disability age 14 and over are eligible for an annual review. Learning difficulties are not the same and patients with learning difficulty will not be eligible for an annual review.
A learning disability is a neurological condition that affects a person’s ability to process, understand, or retain information, which can make it challenging for them to learn new things or perform certain tasks. A learning disability will affect the way people learn new things throughout their life; it is a lifelong condition. Learning disabilities usually start in childhood but may not get diagnosed until adulthood. People with a learning disability may need support with understanding complex information, engaging with other people, and developing new skills.
Approximately 1.5 million people have learning disabilities in the UK.
Why is it important to attend an annual review?
Learning from Lives and Deaths (LeDeR), reviews deaths to see where we can find areas of learning, opportunities to improve, and examples of excellent practice. This information is then used to improve services for people living with a learning disability and autistic people.
Ledar Action from Learning each year around 41% of the Learning Disabilities UK population die of preventable diseases, according to LeDeR (Learning Disabilities Mortality Review NHS England), people with a learning disability often experience poorer health compared with the general population. The review investigates the deaths of people with a learning disability and revealed that on average, they die 20 years earlier than the rest of the population. They are also three times more likely to die from avoidable causes.
In 2006, the Disability Rights Commission recommended the introduction of annual health checks for people living with a learning disability in England and Wales.
Annual health checks are designed to promote healthy living and wellbeing, identify health issues early.
Useful links and easy read health information.
Get checked out – Learning Disability Service easy read format annual review information
learningdisabilityservice-leeds.nhs.uk
https://www.learningdisabilityservice-leeds.nhs.uk › get…
A safe space
The Compton Centre community hub. Harehills Lane Leeds LS9 … The building is a ‘Safe Place‘ for adults with a learning disability.
https://www.leeds.gov.uk › community-hubs › compton-…
Local learning disability groups and support services.
Learning Disability & Autism – People in Action (Yorkshire)
Leep1 – Supporting adults with learning disabilities to speak
Leeds Mencap – Learning Disability Charity – Leeds Mencap



Role of PCN Dietitian
The PCN Dietitian is a member of the healthcare team who works with GP practices within the PCN. The dietitian service is available for all 12 practices in the BHR PCN for adults aged 18 and over. Our PCN’s focus areas are Diabetes and Obesity.
Diabetes
The Dietitian can provide you with individualised dietary information to help you manage your diet better and improve your diabetic control to reduce your risk of diabetic complications.
The dietitian will work with you to improve your knowledge and confidence by devising a dietary plan, setting goals and reviewing your progress.
Who can see the PCN Dietitian?
- Adults aged 18 years plus.
- You have a diagnosis of Type 2 diabetes with confirmed HbA1c >58, and have had at least one assessment with your GP and/or Practice Nurse and need a dietary review to improve your HbA1c.
- You have newly diagnosed Type 2 Diabetes (within the last 6 months) with HbA1c>48.
- You are on multiple medications or insulin, but have high HbA1c
- You need carbohydrate awareness education.
- You are frail with Type 2 diabetes and need dietary advice.
- You need weight management advice
- You have had diabetes for less than 6 years and are interested in the type 2 diabetes remission programme or support
- You are commencing GLP1 medications (You will need a diabetes medication review before starting the diet – we will liaise with relevant staff).
- You do not engage with the specialist teams or other services.
You are NOT suitable if:
- You are under 17 years of age.
- You have Type 1 diabetes and are under a specialist hospital team.
- You are actively under the Leeds diabetes community team.
Weight Management
The Dietitian can support you to build the knowledge, confidence and skills to achieve your health and weight management goals.
Who can see the PCN Dietitian?
- Adults aged 18 years plus.
- You need weight management and have a BMI >35.
- You have a BMI>35 with a Long Term Condition (LTC).
- You have a BMI>35 with Polycystic Ovary Syndrome (PCOS).
You are NOT suitable if:
- You are under 17 years of age.
- You are actively under a specialist weight management team.
- You have other dietary conditions except diabetes and obesity as a co-morbidity.
How to Book
- You can schedule appointments directly with the dietitian without needing a GP consultation or referral.
- You can book into the PCN dietitian clinic appointment slots on the Confed Hub. Book directly on SystmOne dietitian clinic rota on the GP Conf Hub (under Nusrat Kausar).
Patient Information Sheet to see PCN Dietitian
Role of PCN Dietitian
The PCN Dietitian is a member of the healthcare team who works with GP practices within the PCN in your local area. They can provide you with individualised dietary information to help you manage your diet better and improve your diabetic control, to reduce your chance of developing other health problems due to your diabetes. For patients with weight management needs, they can support you to build the knowledge, confidence and skills to achieve your health and weight management goals.
They will discuss your food and drink in detail and work with you to improve your knowledge and help you to manage your diabetic diet better or manage your diet to support weight loss and reduce your chance of developing other health problems due to your weight. They will help you put together a dietary plan and set goals that you can work towards and then review your progress.
At your first appointment you will have a 45-minute telephone or face-to-face assessment and the Dietitian will decide the best way forward to review your progress. If appropriate, a further 30-minute follow up appointment will be arranged for you.
Who can see the PCN Dietitian?
Adults aged 18 years plus.
For Diabetes:
- You have a diagnosis of Type 2 diabetes with confirmed HbA1c over 58, and have had at least one assessment with your GP and/or Practice Nurse and need a dietary review to improve your HbA1c.
- You have newly diagnosed Type 2 Diabetes (within the last 6 months) with HbA1c>48.
- You are on multiple medications or insulin but have high HbA1c.
- You need carbohydrate awareness education.
- You are frail with T2DM and need dietary advice.
- You need weight management for T2DM optimisation including T2 Remission support, Low or very low carb diet, Low calorie diet, or are commencing GLP1 medications.
- You do not engage with specialist teams or other services.
For Weight Management:
- You need weight management and have a BMI over 35.
- You have a BMI>35 with a Long Term Condition (LTC).
- You have a BMI>35 with Polycystic Ovary Syndrome (PCOS).
Nusrat Kausar works a hybrid model; face-to-face consultation on a Tuesday, based at HC2 and remotely on a Friday.
- To book an appointment with the dietitian, please see rotas in the GP Confed hub
- You can book in for face-to-face appointments (on Tuesdays) or telephone appointments ONLY (on Fridays).
- You can schedule appointments directly with the dietitian without needing a GP consultation or referral. Just ask at reception.
Community NHS health checks
The Health Population Management Hub are currently offering NHS health checks at community events in the area to patients who are eligible and registered within the 12 practices.
What is an NHS health check?
The NHS Health Check is a free check-up of your overall health. It can tell you whether you’re at higher risk of getting certain health problems, such as:
- Heart disease
- Diabetes
- kidney disease
- Stroke
If you’re aged over 65, you’ll also be told about symptoms of dementia to look out for.
Are you Eligible?
The check is for people who are aged 40 to 74 who do not have any of the following pre-existing conditions:
- Heart disease
- Chronic kidney disease
- Diabetes – pre diabetes
- High Blood Pressure (hypertension)
- Atrial Fibrillation
- Transient ischaemic attack
- Inherited high cholesterol (familial hypercholesterolemia)
- Heart failure
- Peripheral arterial disease
- Stroke
Or currently being prescribed statins to lower cholesterol
What Happens during an NHS health check
During your NHS health check the following will happen
- Height, weight and waist measurement
- Blood pressure reading
- Cholesterol test using Point of care testing.
- Family history
- Diet and lifestyle questions.
All of this helps to work out your Q-risk score. This will tell you your risk of developing cardiovascular disease in the next 10 years.
What is point of care testing?
Point of care testing is a type of test that allows for immediate results.
A small sample of blood is taken from the finger. The test is then analysed, and results are available within a short period of time.
Watch our video to find out more about what happens during a community NHS health check.
Change in weight management treatment referral criteria from 29 July 2025
From Tuesday 29 July 2025 entry requirements across all weight management services in West Yorkshire will follow that of Tirzepatide (Mounjaro). The access criteria for cohort/year 1 is:
- 1. BMI ≥ 40 (adjusted for ethnicity) AND at least four of the following type 2 diabetes
- 2. Hypertension
- 3. Cardiovascular disease
- 4. Obstructive sleep apnoea
- 5. Dyslipidaemia
- 6. OR where weight loss is needed for life saving and urgent surgery or intervention.
This follows the development of West Yorkshire ICB’s commissioning policy for weight management treatment pathways, aligning them to the Tirzepatide prescribing guidelines issued by NICE and NHS England.
More information is available here: https://www.wypartnership.co.uk/our-priorities/weight-management-west-yorkshire
The Leeds Specialist Weight Management Service (SWMS) has reviewed all of its referral guidance and information to support this change and also updated Leeds Health Pathways:
Specialist Weight Management clinic (Leeds patients only)
What this means for referrals
Since the SWMS reopened to accept new referrals, it has received more referrals than anticipated and is exploring how to manage those that do not meet the new criteria.
Anyone referred who does not meet the criteria given above will not be accepted by the SWMS.
We are exploring alternative primary care offers and integrated pathways to increase capacity and to support primary care. We will provide further updates as this progresses.
Primary care prescribing in Leeds
Prescribing may only occur in commissioned weight management services. Currently only practices in four Primary Care Networks (PCNs) in Leeds can prescribe injectable weight management medications to a limited number of patients as part of a feasibility study until April 2026:
- Burmantofts, Harehills and Richmond Hill
- Beeston
- Crossgates
- West Leeds
The information gathered will inform the approach taken to primary care prescribing of weight management medication in Leeds.
Further information will follow, but if you have any further queries, please contact wyicb-leeds.primarycare@nhs.net

